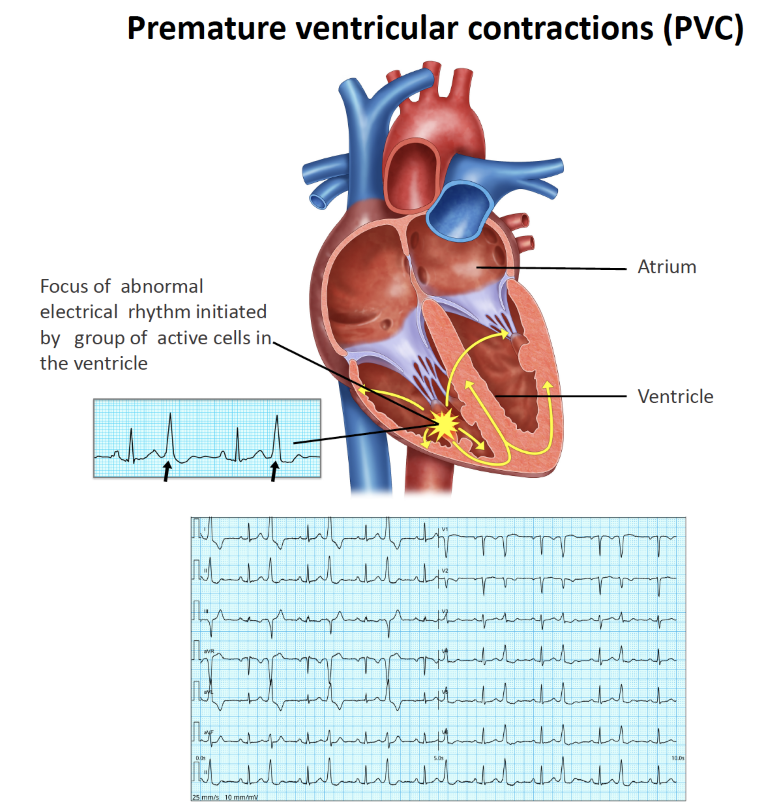
Premature ventricular contractions (PVC)
What is a premature ventricular contraction (PVC)?
Each individual cell within the heart possesses the inherent ability to contract and initiate a heartbeat. Occasionally, certain cells or groups of cells may exhibit premature contractions. When these untimely beats originate from the lower chamber (ventricle) of the heart, the condition is referred to as Premature Ventricular Contraction (PVC), also known as ventricular ectopy (VE).
These additional beats disrupt the regular rhythm of the heart, leading to symptoms such as palpitations, skipped beats, dropped beats or fluttering sensations. It is important to note that experiencing occasional extra beats is considered normal, and nearly everyone experiences them. However, when a significant number of extra beats occur, accompanied by symptoms or a weakening of the heart muscle, treatment may be necessary. The frequency and intensity of these extra beats can vary, with some days being better than others. It is common for individuals to notice these extra beats more often when at rest, particularly during night-time hours. During daytime activities, the presence of distractions often makes them less noticeable. It is also worth mentioning that extra beats can arise from multiple locations within the heart. When the majority of PVCs originate predominantly from a single location, it is referred to as monomorphic or predominantly monomorphic PVC. Conversely, if multiple sources are observed, it is termed multifocal PVC.
What are the consequences of PVC?
In the majority of individuals, premature ventricular contractions (PVCs) are generally not considered dangerous and have little clinical significance. The quantity of PVCs, your symptoms, and the overall condition of your heart are the primary factors that will determine the appropriate course of action. In a healthy individual with low burden PVC, no monitoring is required. In many cases, only monitoring is necessary.
It’s important to note that your heart beats approximately 100,000 times per day. When PVCs exceed 10-20% of these beats (more than 10,000-20,000 beats), it may have clinical implications. Some individuals are highly sensitive and can feel each PVC, which can be distressing. However, when the total burden of PVCs is low (less than 5%), it is unlikely to have any clinical consequences. On the other hand, a high burden of PVCs (more than 20%) can potentially lead to a weakening of the heart muscle, known as PVC-induced cardiomyopathy, and monitoring is necessary to detect this condition.
In certain individuals, PVCs can cause troublesome symptoms such as palpitations, decreased energy, shortness of breath, and reduced exercise capacity. It is important to differentiate PVCs, which are single premature beats, from a fast and continuous rhythm called ventricular tachycardia (VT). VT can result in severe symptoms such as dizziness, shortness of breath, palpitations, and chest pain. In individuals with a structurally normal heart, VT is considered a treatable condition.
While rare, PVCs may have more concerning implications, particularly in individuals with coexisting heart problems. They can potentially trigger malignant abnormal rhythms.
Is PVC dangerous?
In individuals with a normal heart, the presence of low burden PVCs is not typically considered life-threatening. However, when PVCs occur at a higher burden, they can potentially contribute to the development of cardiomyopathy. In such cases, it is recommended to undergo periodic screening, such as infrequent echocardiograms and 24-hour Holter monitoring, to monitor the condition over the long term. These screening measures aim to assess the impact of PVCs on the heart and ensure early detection of any potential cardiomyopathy.
Where do they come from?
While premature ventricular contractions (PVCs) can originate from various regions within the ventricles, there are specific sites that tend to be more commonly involved. These include the right ventricular outflow tract, left ventricular outflow tract, left ventricular summit, papillary muscles, mitral annulus, and tricuspid annulus. By capturing the PVCs effectively on a 12-lead ECG, it may be possible to identify the specific site from which they originate. Determining the origin of PVCs can have implications for planning appropriate therapeutic interventions, such as ablation, if necessary. Understanding the specific site of origin can help guide the treatment approach to effectively manage PVCs.
How can I prevent PVCs / VEs?
PVCs or VEs can be aggravated by various common factors, including sleep deprivation, medical illnesses, and electrolyte imbalances such as low magnesium levels and dehydration. However, it’s important to recognize that each individual may have unique factors that specifically exacerbate their PVCs. In general, maintaining sufficient sleep, staying hydrated, and avoiding stimulants can help prevent the worsening of PVCs. It’s worth noting that PVCs are not always predictable and may occur randomly, making it challenging to anticipate their occurrence.
What is the long-term prognosis with PVC?
The vast majority of individuals with PVCs can anticipate leading a normal, healthy life if the burden of PVCs is low and the heart structure is normal. However, if you have a high burden of PVCs, experience multifocal PVCs, or have cardiomyopathy, your prognosis may vary. For those who require treatment, the prognosis is significantly enhanced with the availability of modern medications and, if necessary, an ablation procedure. These advancements in medical interventions contribute to improved outcomes and quality of life for individuals with PVCs requiring intervention.
What are the treatment options available for PVC?
Conservative management:
If you have a good understanding of your PVC, it is of low burden without severe symptoms and a structurally normal heart, you can choose not to have any treatment. Treatment is often not recommended.
Medications:
Medications are the primary and most commonly used form of treatment for the majority of cases with significant burden or troublesome symptoms related to PVCs. In many individuals, medications prove to be highly effective. However, for those who continue to experience PVC episodes despite medication use, have difficulties with tolerating prescribed medications, or prefer to avoid long-term medication use, procedural options can be explored. Multifocal PVCs, in particular, are generally managed with medication-based treatments.
Procedural options:
Catheter ablation is a commonly performed minimally invasive procedure aimed at identifying and eliminating abnormal foci to prevent the recurrence of PVCs. The success rate of the procedure can vary depending on the specific sites targeted, but generally falls within the range of 80-95% with one or two procedures.

PVC ablation is typically reserved for individuals with monomorphic or predominantly monomorphic PVCs, occurring at a significant burden (usually exceeding 10%), who experience symptoms or have cardiomyopathy. The procedure is offered to those who have not achieved satisfactory results with medical therapy or who cannot tolerate medication. Younger individuals often opt for ablation to avoid the lifelong reliance on medications.
By undergoing ablation, individuals seek to mitigate the need for long-term medication use and improve their overall quality of life.